Introduction:
It is important to point out that typhoid fever is caused by the bacterium Salmonella, which remains a significant global health concern, particularly in regions with poor sanitation and limited access to clean water.
One of the severe complications of typhoid fever is typhoid bleeding, characterized by active bleeding from the intestines, which can lead to death if not handled well by medical experts.
I have created this post to create awareness about the best way to avoid typhoid bleeding by timely treating typhoid fever and instituting proper hand hygiene, usage of clean water, and sanitation.
The main challenge is that typhoid fever is worse in children and a lot is needed to enhance the hygiene condition of children.
What is typhoid bleeding?
Typhoid bleeding, also known as intestinal hemorrhage, is a severe and potentially life-threatening complication of typhoid fever, a systemic infection caused by the bacterium Salmonella serotype Typhi. This complication typically occurs during the second to fourth week of untreated or inadequately treated typhoid fever and is characterized by blood loss, primarily originating from the gastrointestinal tract.
How Typhoid Bleeding Happens:
Typhoid bleeding typically occurs during the second to fourth week of untreated or inadequately treated typhoid fever. Many factors contribute to this intestinal bleeding from typhoid fever and they include how strong and destructive the bacteria species is in causing disease, how far your body can go in fighting the infection, and also how healthy your blood vessels are.
Salmonella typhi, the bacteria that cause typhoid fever, enters your intestinal mucosa after entering through your mouth with contaminated food or water. It then disseminates through the bloodstream, leading to systemic infection. Within the body, Salmonella typhi exhibits various actions to cause diseases, including the production of outer membrane proteins, lipopolysaccharides, and exotoxins, which contribute to tissue damage and immune evasion.
One of the hallmark features of typhoid fever is the formation of typhoid nodules, which are aggregates of macrophages, lymphocytes, and bacteria in the intestinal mucosa and lymphoid organs. These nodules serve as reservoirs for bacterial replication and dissemination. Additionally, Salmonella Typhi can invade the endothelial cells lining the blood vessels, leading to endothelial dysfunction and microvascular injury.
The host immune response to Salmonella infection plays a crucial role in the pathogenesis of typhoid bleeding. Dysregulated immune activation, characterized by the release of pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6), contributes to endothelial activation and increased vascular permeability. This pro-inflammatory state, combined with direct bacterial damage to the vascular endothelium, predisposes individuals to bleeding diathesis.
Furthermore, thrombocytopenia, a common hematological manifestation of typhoid fever, exacerbates the risk of bleeding complications. Platelet dysfunction, consumption, and sequestration within the spleen contribute to impaired hemostasis and increased susceptibility to hemorrhage.
Risk Factors for Typhoid Bleeding:
Several factors influence the development and severity of typhoid bleeding. These include:
- Delayed or inadequate treatment of typhoid fever: Prolonged bacterial dissemination and systemic inflammation increase the risk of vascular damage and hemorrhage.
- Disease severity: severe forms of typhoid fever, characterized by a high bacterial load, profound immune activation, and multi-organ involvement, are associated with a higher incidence of bleeding complications.
- Coagulation abnormalities: Pre-existing coagulopathies or underlying conditions such as liver disease may exacerbate bleeding tendencies in patients with typhoid fever.
- Age and immune status: Children and immunocompromised individuals are at increased risk of developing severe typhoid fever and subsequent complications, including typhoid bleeding.
Clinical Manifestations of Typhoid Bleeding:
Typhoid bleeding can manifest in various forms, ranging from mild gastrointestinal bleeding to life-threatening disseminated intravascular coagulation (DIC). Common clinical presentations include:
- Gastrointestinal bleeding: Hematochezia (bloody stools) or melena (dark, tarry stools) may occur due to intestinal ulceration and mucosal damage caused by Salmonella typhi.
- Hematemesis: Vomiting of blood may occur secondary to gastric or esophageal ulceration.
- Petechiae and ecchymosis: Small, pinpoint hemorrhages (petechiae) or larger purplish patches (ecchymosis) may appear on the skin due to thrombocytopenia and microvascular damage.
- Hematuria: Blood in the urine may indicate renal involvement and vascular injury.
- Disseminated intravascular coagulation (DIC): In severe cases, widespread activation of the coagulation cascade and consumption of clotting factors can lead to DIC, resulting in uncontrolled bleeding and organ failure.
Treatment of Typhoid Bleeding:
The management of typhoid bleeding requires a multidisciplinary approach involving supportive care, antimicrobial therapy, and hemostatic interventions.
- Fluid resuscitation: Intravenous fluids should be administered to maintain adequate perfusion and electrolyte balance, particularly in patients with hypovolemic shock due to hemorrhage.
- Antimicrobial therapy: prompt initiation of appropriate antibiotics is essential to eradicate the underlying Salmonella infection and prevent disease progression. First-line antibiotics for typhoid fever include fluoroquinolones (e.g., ciprofloxacin) and third-generation cephalosporins (e.g., ceftriaxone). In regions with high rates of antibiotic resistance, alternative agents such as azithromycin or meropenem may be used.
- Blood transfusion: Patients with severe bleeding or DIC may require blood products, including packed red blood cells, platelets, and fresh frozen plasma, to correct coagulopathy and restore hemostasis.
- Proton pump inhibitors (PPIs): PPIs such as omeprazole or pantoprazole may be administered to reduce gastric acid secretion and promote the healing of gastrointestinal ulcers.
- Supportive care: Close monitoring of vital signs, fluid balance, and hematological parameters is essential in the management of typhoid bleeding. Intensive care unit (ICU) admission may be warranted for patients with hemodynamic instability or organ dysfunction.
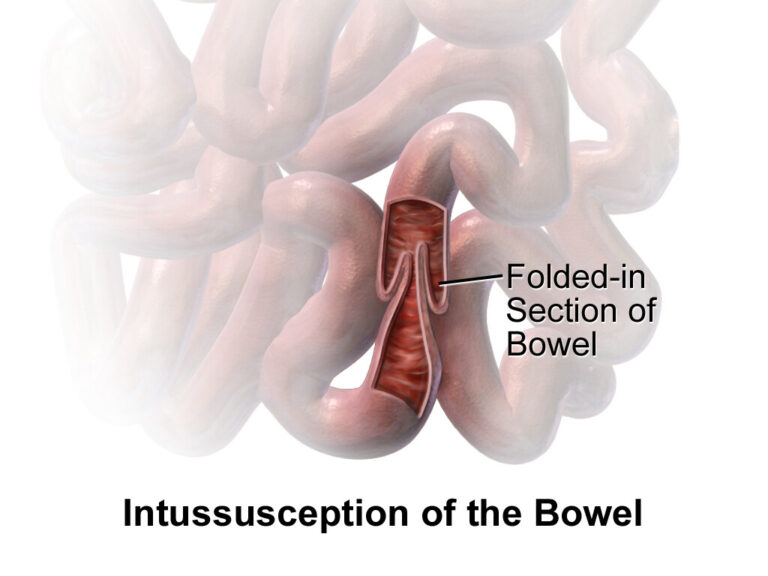
- Surgical intervention: In cases of refractory hemorrhage or complications such as perforation or intestinal obstruction, surgical consultation should be sought for potential endoscopic or operative intervention.
Conclusion:
Typhoid bleeding is a serious and potentially life-threatening complication of typhoid fever, resulting from a complex interplay of bacterial virulence, host immune response, and vascular dysfunction. Early recognition and appropriate management are paramount in reducing morbidity and mortality-associated