Introduction
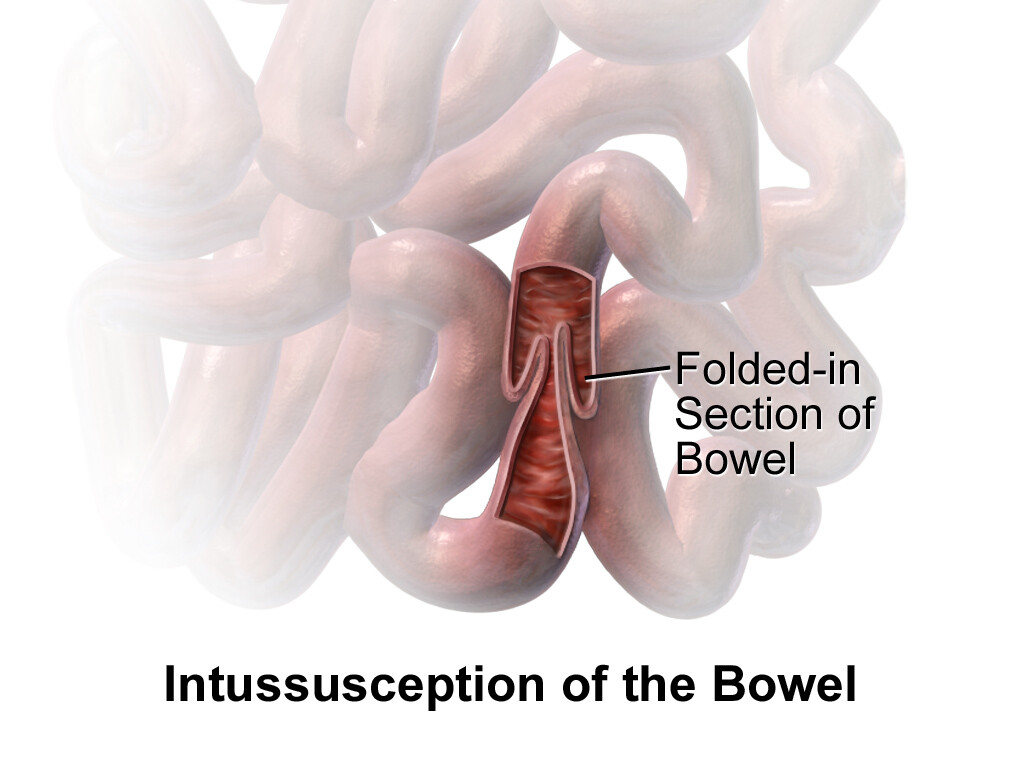
Intussusception is a serious medical condition that occurs when one portion of the intestine invaginates, or telescopes, into an adjacent segment. Normally, breast milk or food taken through the mouth goes out as feces through the anus.
However, before it reaches the anus, it will pass through the intestine after digestion in the stomach takes place. In the case of intussusception, this does not occur because the intestine is blocked by the part that folds inside, just like a telescope folds inside itself.
It predominantly affects infants and young children between three months and three years. It can also occur in adults as well, but less frequently. Understanding the causes, risk factors, how it occurs, and management of intussusception is crucial for prompt diagnosis and appropriate treatment.
Causes of intussusception:
The exact cause of intussusception is often unknown, particularly in infants and young children. However, in many cases, it is associated with a preceding viral infection of the respiratory and gastrointestinal tract, such as adenovirus, rotavirus, or enteric adenovirus. These infections can lead to inflammation and swelling of the intestinal walls, predisposing them to telescoping. Other causes in infants can include early weaning off of breast milk and the early introduction of adult feeds. In adults, causes may include tumors, polyps, or other structural abnormalities within the intestine.
Risk Factors:
Intussusception is becoming common in our society and it is important to note some of the risk factors. Several factors increase the risk of intussusception, including:
- Age: Intussusception primarily affects infants between the ages of 5 and 9 months, with the majority of cases occurring before the age of 3. However, it can occur at any age, including in adults. In adults, intussusception is often associated with an underlying pathological condition, such as a tumor or polyp.
- Previous history: Individuals with a history of intussusception are at an increased risk of recurrence. However, this does not mean that anyone who has had intussusception should be prepared to have it again.
- Sex: It is more prevalent in males.
- Congenital abnormalities: Certain congenital conditions, such as cystic fibrosis or Meckel’s diverticulum, may predispose individuals to intussusception.
- Recent gastrointestinal infection: Viral infections of the gastrointestinal tract can trigger episodes of intussusception, particularly in children. This is why it is important to manage your child in the hospital whenever you notice that they are making watery stools with a fever associated with them.
- Lymphatic hyperplasia: Conditions associated with excessive growth of lymphatic tissue in the intestine, such as Henoch-Schönlein purpura, can increase the risk of intussusception.
Rotavirus vaccine and Intussusception
The Rotavirus vaccine was first considered to be associated with intussusception. This led to the disbandment of the first rotavirus vaccine produced. However, the second rotavirus vaccine has been confirmed not to be associated with intussusception. In some regions, intussusception is seen as rare and seasonal, often associated with either a respiratory tract infection or a gastrointestinal tract infection.
How does intussusception occur?
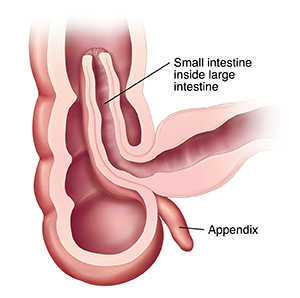
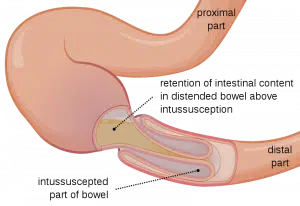
Intussusception involves the telescoping of one segment of the intestine, called the intussusceptum, into an adjacent segment, known as the intussuscipiens. This leads to obstruction of the bowel, impaired blood flow, and compression of the venous and lymphatic vessels within the affected segment.
A segment of the intestine enters, invaginates, or telescopes into an adjacent segment. You know how a telescope enters inside itself? That is how the small intestine enters the adjacent segment. It will lead to obstruction of the bowel, which will lead to impaired blood flow and damage of the segment of the bowel that folds inside. This can result in severe abdominal pain, vomiting, and bloody stools. With these symptoms gradually setting in, the child may no longer tolerate feeding, including water. This can lead to dehydration and hypoglycemia, requiring immediate attention.
The classic triad of symptoms includes severe abdominal pain, vomiting, and bloody stools. However, not all patients present with these symptoms, especially infants, who may only exhibit irritability, lethargy, or inconsolable crying.
It is important to note that if immediate action is not taken, this condition can get worse, leading to more deterioration in your child’s condition. It can also lead to the death of your child if left untreated and within the appropriate time.
Management (diagnosis and treatment)
The management of intussusception depends on several factors, including the age of the patient, the severity of symptoms, and the presence of complications. Treatment options may include:
Home Remedy
When you notice that your child has pain or fever, you can attempt to give a painkiller like paracetamol. This is customary in most families, where mothers give first aid before going to the hospital. However, when you give the paracetamol and it looks like no change is happening, it is important to reach out for urgent hospital care for your child before you lose him or her.
Hospital care
Resuscitation of the child
When you bring your child to the hospital, the first thing the doctor will do is resuscitate your child by giving intravenous fluid, some antibiotics, and painkillers. The reason for this is to stabilize your child while needed investigation is being carried out. Since the intestine is blocked and your child is refusing to feed, this fast resuscitation will ensure that your child receives adequate glucose and other needed nutrients intravenously. Passing a Nasogastric tube through the nose to decompress the stomach can also be done. The urine output can also be monitored by passing a urinary catheter. All these add to better outcomes.
Fluid resuscitation: Patients with intussusception often present with dehydration due to vomiting and fluid loss. Intravenous fluids will be administered to correct dehydration, and possible hypoglycemia and maintain electrolyte balance.
Pain management: Severe abdominal pain is a hallmark symptom of intussusception. Analgesic medications, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), may be prescribed to alleviate pain and discomfort.
Antibiotic therapy: In cases where there is evidence of bacterial infection or peritonitis, antibiotic therapy may be initiated to prevent systemic infection and promote healing.
Radiological investigations
At the hospital, it is important to confirm the diagnosis using radiological and laboratory investigations. If you notice the problem very early, you may take your child for an abdominopelvic ultrasound or a plain abdominal X-ray before visiting the hospital. This will make the doctor act fast in combination with details from history-taking and examination since intussusception is a medical emergency. However, because of the importance of stabilizing the child, it is advised to visit the hospital first, where important investigations may be requested later.
Also, for people living in Nigeria, where there are poor resources in rural areas, ultrasounds and X-rays may not be readily available. Therefore, your doctor may depend solely on his expertise to attend to your child.
Laboratory investigations
Necessary laboratory investigations may include the full blood count and serum electrolyte, urea, and creatinine levels. The doctor may also decide to include other investigations deemed helpful.
Treatment plan:
Non-operative reduction: In many cases, especially in children, intussusception can be successfully managed with non-operative reduction, also known as pneumatic or hydrostatic reduction. This involves using air or liquid enemas under radiological guidance to gently push the telescoped segment of the intestine back into its normal position. In this case, there is no surgical intervention and the patient may be discharged from hospital soon. However, there are more chances of recurrence with this method of care compared to surgical intervention.
Surgical intervention: If non-operative reduction fails or if there are signs of bowel perforation, ischemia, or peritonitis, surgical intervention may be necessary. The surgical procedure, known as laparotomy, involves making an incision in the abdomen to manually reduce the intussusception and inspecting the bowel for any signs of damage or pathology.
In this case, the surgeon will open the abdomen and look at the intestine to find out all the problems involved. It may involve finding out the problem and removing the damaged part of the intestine. In some cases, it involves pushing out the part of the intestine that entered into its adjacent segment and then closing the abdomen.
Note: The best treatment plan is made by your doctor depending on what is observed from the combination of history-taking, examination findings, and investigation results. Whichever decision is made, this condition is a medical emergency that needs immediate attention.
Monitoring: After successful reduction or surgical intervention, patients are typically monitored closely for signs of recurrence, bowel obstruction, or other complications. In many cases, the child may be allowed to stay for days in the hospital until the post-operative condition is deemed fit for the child to go home.
Complications
- Reoccurrence
- Affects the absorption of some nutrient
- Fistula formation
- Anastomosis breakdown
Conclusion
Intussusception is a serious medical condition characterized by the telescoping of one portion of the intestine into another, leading to bowel obstruction and impaired blood flow. While it primarily affects infants and young children, it can also occur in adults. Prompt diagnosis and appropriate management, including non-operative reduction or surgical intervention, are essential for optimizing outcomes and preventing complications.